World AIDS Day on December 1 is an opportunity to reflect on the spectacular progress made towards preventing and treating HIV — but a cure for the virus 39 million people are currently living with remains elusive.
While antiretroviral therapy (ART) for HIV stops the virus from replicating, stops people from getting sick and stops a person with HIV from infecting others, treatment for people with HIV must be continued for life.
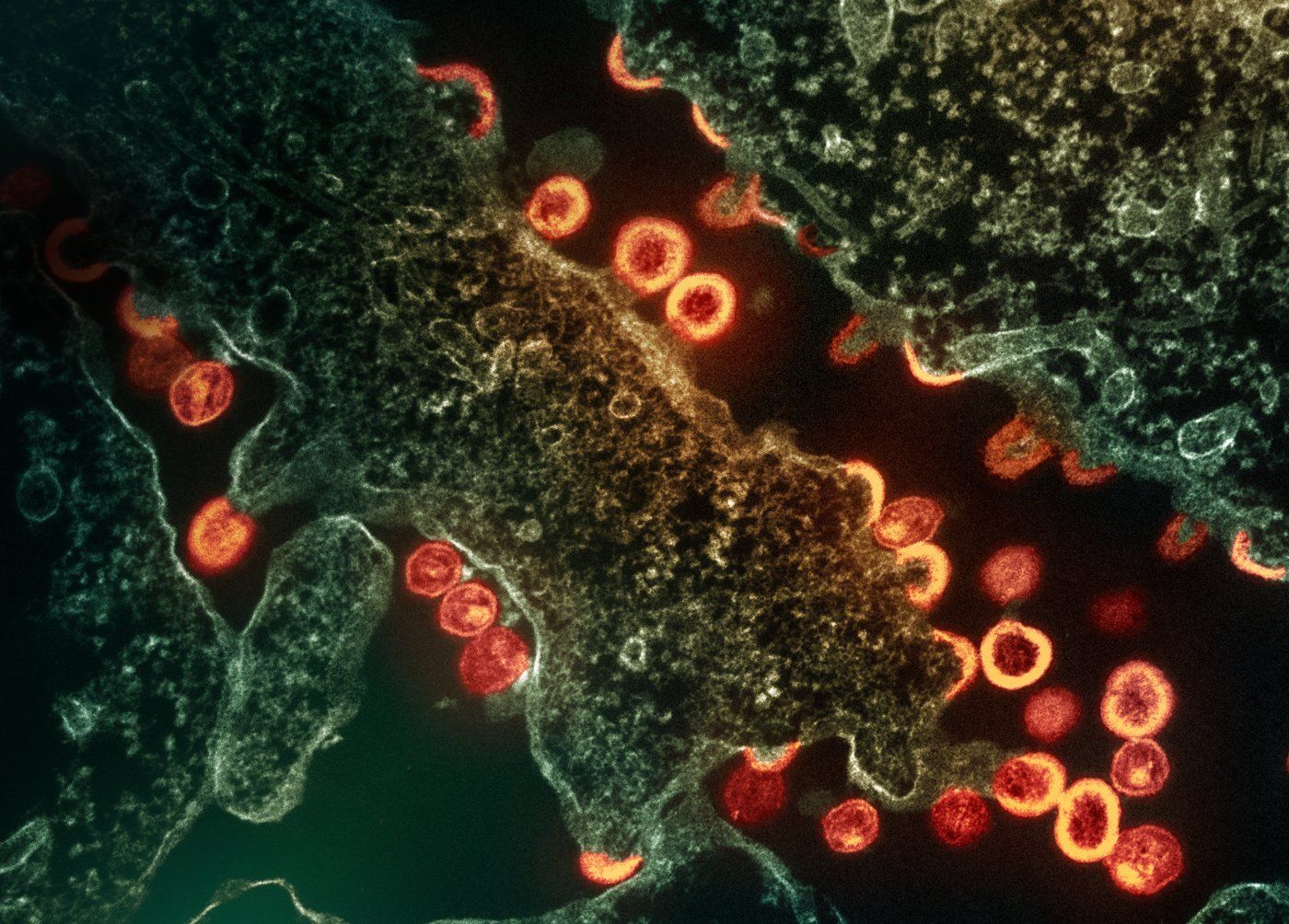
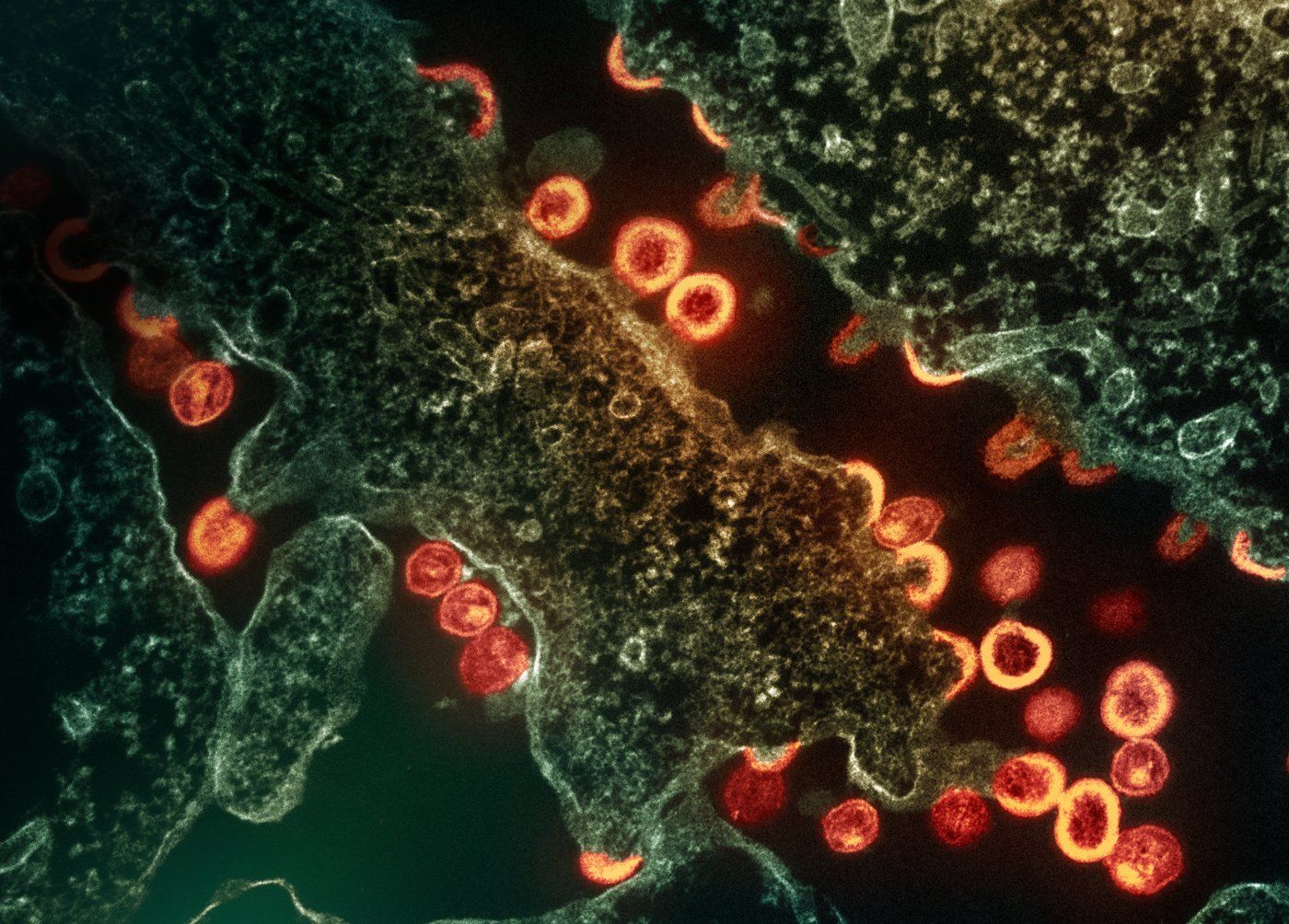
ART doesn't cure HIV because the virus has a sneaky trick: it can hide and become inactive, a state known as latent infection.
Once a person stops treatment, the latent virus becomes active again and resumes replication.
But drawing on advances in cancer treatment, gene editing and mRNA technology, researchers continue to make significant strides in pursuit of an HIV cure.
Globally, scientists are actively developing and testing interventions that specifically tackle latent virus, with the eventual goal to achieve virus-free control after stopping antiviral treatment.
HIV cure: from the theoretical to the possible
In the 40 years since the discovery of the virus, complete eradication and cure of HIV have been achieved in six exceptional cases.
These individuals all underwent stem cell transplants to treat life-threatening blood cancers, with all but one receiving stem cells from donors with a rare genetic trait that makes their cells resistant to HIV.
As a result, all six individuals were able to stop ART after the intervention, and the virus has not reappeared after years of follow-up.
However, due to the high risk of complications associated with stem cell transplant procedures, they are not a viable pathway towards a cure for the broader HIV community. Nonetheless, these cases have shown the world that an HIV cure is possible.
Approaches to safely stopping ART: reduce and control
Several therapeutic strategies are under investigation to reduce and control the latent HIV reservoir, without the need for invasive stem cell transplants.
One approach seeks to find treatments that force the latent virus out of its hidden, inactive state.
This process of reactivation can result in the death of the infected cell or its recognition and elimination by the immune system. This can be done safely, preventing nearby cells from becoming infected, by activating the virus while the person with HIV is on ART.
An alternative strategy involves the use of drugs to drive the persisting virus into further hiding.
In this permanent state of latency, the virus remains dormant and can never be reactivated. While this approach does not eradicate the pool of infected cells, it would mitigate the risk of the virus re-emerging when ART is stopped.
Both these approaches are still under development so are not yet being used in the clinic.
Other approaches aim to enhance the immune system's ability to control HIV, in the absence of antiretroviral therapy.
Recent small-scale clinical trials have shown that boosting immune function with HIV-specific antibodies or an HIV vaccine can allow approximately one third of participants to stop ART for a defined period and still keep the virus under control.
While these are very encouraging findings, larger trials are needed, along with a better understanding of why and how some participants can sustain virus control while others cannot.
Learning from new treatments for cancer that boost immunity
HIV researchers are also learning from new therapies being deployed to fight cancer.
Immunotherapy has revolutionized cancer treatments. Unlike traditional cancer treatments that poison the tumor itself, this new type of medicine targets the immune system.
One form of immunotherapy, called anti-PD1, has achieved remarkable results in the treatment of certain cancers, by reinvigorating an exhausted immune system.
The immune system of people with HIV also gets exhausted, even with treatment.
Australian researchers have been studying what happens in people with HIV on antiretroviral therapy who also have cancer and receive anti-PD1.
Findings reveal that anti-PD1 can not only wake up the virus directly, but can also reinvigorate the immune system, specifically the components that target HIV.
Studies underway of anti-PD1 in people with HIV on antiretroviral therapy who don't have cancer, are showing promise.
One concern is toxicity, so Australian and Singaporean researchers are leading a study administering anti-PD1 at a reduced dose — ranging from one tenth to one hundredth of the standard dose — to reduce any adverse effects.
Gene editing to specifically delete HIV from infected cells
Another technique being developed is using gene editing to specifically delete HIV from infected cells.
In July 2023, the US Food and Drug Administration granted Fast Track designation for a first-in-class gene therapy, EBT-101.
EBT-101 is designed to 'cut out' and incapacitate HIV within latently infected cells using gene editing, with a Clinical Phase I/II Trial currently underway.
Gene editing is a rapidly changing field, with new technologies enabling the direct injection of the gene-editing machinery in individuals, rather than having to remove cells to process the gene editing outside of the body.
Rigorous monitoring of participants in these trials is essential to ensure no off-target gene editing occurs, where unintentional changes to human DNA occur instead of targeting viral DNA. There is no evidence to date this is happening, but long-term follow-up will be needed.
Beyond targeting the virus itself, the ability for gene editing to make cells resistant to infection or to increase immunity is also being evaluated in clinical trials involving people with HIV on ART.
From COVID vaccine to HIV cure: the potential of mRNA technology
The COVID-19 pandemic allowed for the rapid development of mRNA technology for vaccines, but it could also help in the search for an HIV cure.
This new technology has significant implications for next-generation medicines, which can be delivered by mRNA wrapped in a fat bubble, called a lipid nanoparticle.
These lipid nanoparticles can be designed to reach specific diseased organs or cells, and deliver therapeutics at this precise location.
Researchers are taking advantage of these new ways to deliver gene-editing tools to cure HIV.
A lipid nanoparticle is being developed that can specifically deliver mRNA to a resting T-cell where HIV hides in the body.
The mRNA has been designed to activate the virus, which would then allow it to be knocked out by the person's own immune system. Initial results in test-tube models are promising. The next step will be to test this approach in animal models of HIV.
While the science for finding an HIV cure rapidly advances, people living with HIV around the world remain keen to know when a cure will be available and whether it will be available globally.
Any cure that is developed must be not only effective but also scalable and widely accessible in order to solve the great challenge that is HIV.
(Dr Paula Cevaal is a postdoctoral researcher at the Peter Doherty Institute for Infection and Immunity, working on developing mRNA lipid nanoparticles as therapeutics towards an HIV cure. Dr Michael Roche is a senior research fellow at the Peter Doherty Institute for Infection and Immunity. Professor Sharon Lewin is a leading infectious diseases expert and the inaugural Director of the Peter Doherty Institute for Infection and Immunity. This article was originally published under Creative Commons by 360info)